A podiatrist may treat a diabetic ulcer using a combination of approaches, which can vary depending on the severity and location of the ulcer. Some common treatments include:
Debridement: Removing dead or damaged tissue from the wound to promote healing and prevent infection.
Infection control: Treating any underlying infection with antibiotics or other medications.
Offloading: Reducing pressure on the wound by using padding or special footwear to redistribute weight and relieve pressure on the ulcer.
Wound dressings: Applying specialized dressings that can help keep the wound moist and promote healing.
Blood sugar control: Ensuring that the patient’s blood sugar levels are well-controlled, which can help prevent further damage to the wound and promote healing.
Surgery: In severe cases, surgery may be required to remove damaged tissue or address other issues that are hindering healing.
Patient education: Teaching the patient about proper foot care, including daily foot inspections, maintaining good hygiene, and wearing appropriate footwear.
It’s worth noting that diabetic ulcers can be complex and require ongoing treatment and monitoring. A podiatrist may work closely with other healthcare providers, such as endocrinologists, wound care specialists, and infectious disease specialists, to ensure that the patient receives comprehensive care.
More Details
Debridement: Debridement is the process of removing dead or damaged tissue from the ulcer to promote healing and prevent infection. This may involve using a scalpel, specialized dressings, or other methods. The goal is to create a clean wound bed that is conducive to healing.
Infection control: If the ulcer is infected, the podiatrist may prescribe antibiotics or other medications to treat the infection. They may also clean the wound and apply topical antimicrobial agents to help prevent infection.
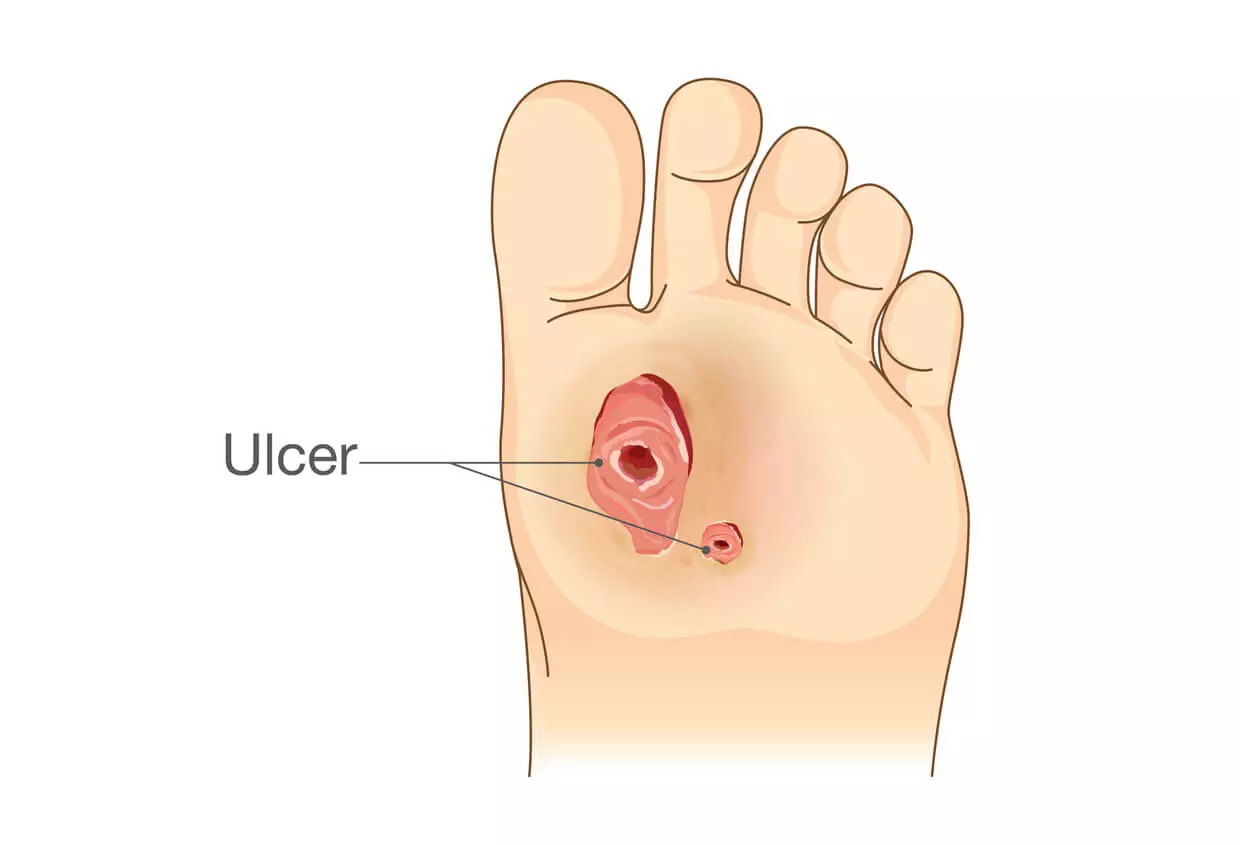
Offloading: Offloading refers to reducing pressure on the wound to promote healing. This can be achieved through the use of padding, specialized footwear, or other devices that redistribute weight away from the ulcer. Offloading may be particularly important for ulcers located on the bottom of the foot, which can be difficult to heal due to the constant pressure placed on them during walking.
Wound dressings: There are a variety of wound dressings that a podiatrist may use to help promote healing of a diabetic ulcer. Some dressings are designed to help maintain a moist wound environment, while others are designed to absorb excess drainage or protect the wound from further damage. The podiatrist may select a dressing based on the location and severity of the ulcer.
Blood sugar control: High blood sugar levels can interfere with wound healing, so it’s important to ensure that the patient’s blood sugar levels are well-controlled. This may involve making dietary changes, adjusting medication dosages, or other strategies to help keep blood sugar levels within a healthy range.
Surgery: In some cases, surgery may be necessary to remove damaged tissue, address underlying bone or joint problems, or address other issues that are hindering healing. The podiatrist may perform the surgery themselves or refer the patient to a specialist.
Patient education: Proper foot care is essential for preventing diabetic ulcers and promoting healing of existing ulcers. The podiatrist may educate the patient on proper foot hygiene, including daily foot inspections, washing and drying feet thoroughly, and wearing appropriate footwear. They may also teach the patient how to monitor their feet for signs of infection or other problems and when to seek medical attention.
Benefits of Seeing a Podiatrist
Here are some of the benefits of seeing a podiatrist for diabetic ulcer treatment and related foot problems:
Expertise: Podiatrists are medical professionals who specialize in diagnosing and treating conditions that affect the feet and ankles. They have extensive training and experience in caring for patients with diabetic foot problems, including diabetic ulcers.
Comprehensive care: Podiatrists can provide comprehensive care for diabetic foot problems, including wound care, infection control, and offloading strategies. They can also help manage underlying conditions, such as neuropathy, that can contribute to foot problems.
Preventative care: In addition to treating existing foot problems, podiatrists can help prevent future foot problems by educating patients on proper foot care and footwear selection.
Collaboration: Podiatrists may work closely with other healthcare providers, such as endocrinologists, wound care specialists, and infectious disease specialists, to ensure that patients receive comprehensive care for their foot problems.
Customized treatment: Podiatrists can develop customized treatment plans for patients based on their individual needs and circumstances. This may include a combination of wound care, offloading strategies, and other interventions to promote healing.
Monitoring: Podiatrists can monitor the progress of a diabetic ulcer or other foot problem over time and adjust the treatment plan as needed to ensure the best possible outcome.
Improved quality of life: By addressing foot problems and preventing future complications, podiatrists can help patients maintain their mobility, independence, and overall quality of life.
In conclusion, diabetic foot ulcers are a serious complication of diabetes that require prompt and effective treatment to prevent further complications. Podiatrists play a critical role in the care of patients with diabetic foot problems, including ulcers. They have the expertise and tools necessary to diagnose and treat foot problems, as well as prevent future complications.
By working closely with other healthcare providers and developing customized treatment plans for each patient, podiatrists can help improve the outcomes and quality of life for patients with diabetic ulcers and related foot problems. If you have diabetes and are experiencing foot problems, it is important to seek care from a podiatrist or other healthcare provider as soon as possible.

Carl Clay is a health blog author who has been writing about nutrition, fitness and healthy living for over 10 years. He also loves to run, hike and bike with her wife.












